- Overview
- Step-by-Step Guide to Compliance
- Flow Chart
- Questions and Answers for Dental Employers
- Reference List
- Additional Links
Employer Obligations After Exposure Incidents (OSHA)
Introduction: A Guide to Employer Obligations
Overview
OSHA's final rule for Occupational Exposure to Bloodborne Pathogens [29 CFR 1910.1030(f)] requires the dental employer to make immediately available confidential medical evaluation and follow-up to an employee reporting an exposure incident. An exposure incident is any eye, mouth, mucous membrane, non-intact skin, or other parenteral contact with blood or other potentially infectious material (OPIM). (For example, a puncture from a contaminated sharp such as an injection needle or a cut from a scalpel blade or suture needle.) Saliva in dental procedures is treated as OPIM.
The dental employer must refer the exposed employee to a licensed health care professional. This means a person who is licensed under the laws of the state where he/she practices to independently provide the post-exposure evaluation and follow-up services required by the standard. The health care professional will counsel the individual about what happened and how to prevent further spread of any potential infection. He or she will prescribe appropriate follow-up in accordance with current U.S. Public Health Service recommendations. The licensed health care professional also will evaluate any reported illness to determine if the symptoms may be related to Human Immunodeficiency Virus (HIV) or Hepatitis B Virus (HBV) infection.
Note: The standard is designed to prevent occupational exposure to blood or OPIM. If the required controls are in place and the standard is correctly implemented, then exposure incidents will be relatively uncommon events.
Step-by-Step Guide to Compliance
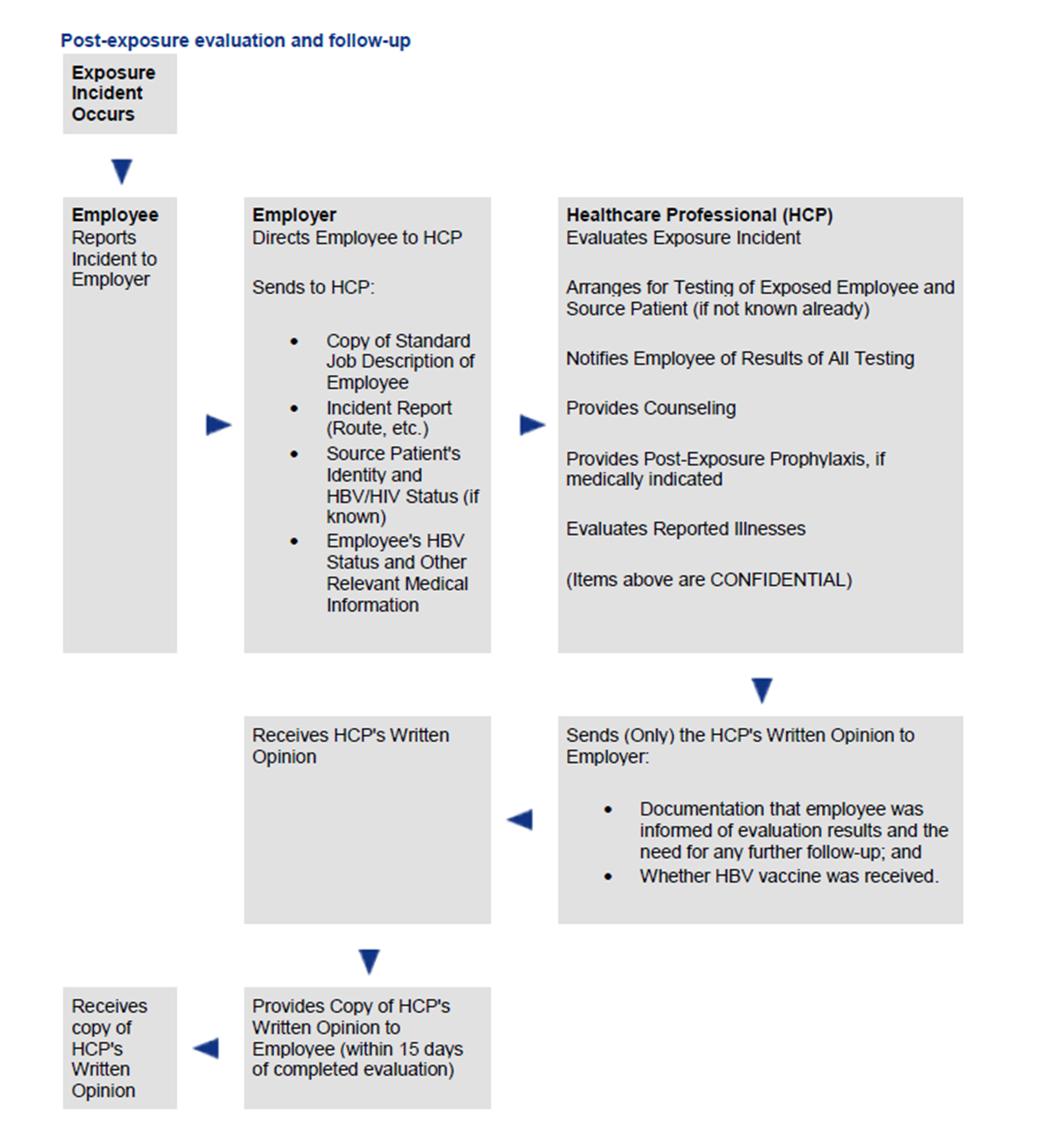
This section is designed to supplement the flow chart outlining the standard's requirements following an exposure incident.
Flow Chart
A flow chart providing visual step-by-step guidance to the standard's requirements for post-exposure evaluation and follow-up.
Questions and Answers for Dental Employers
Sample "questions and answers" addressing potential dental employer concerns.
Reference List
A Reference List, including OSHA publications, as well as relevant CDC guidelines and recommendations.
Additional Links
Internet resources containing information for health care professionals on infection control and occupational safety.
A Step-by-Step Guide to Compliance
Note: This section is designed to supplement the flow chart outlining the standard's requirements following an exposure incident.
- Reporting Incident
- Referral to a Health Care Professional (HCP)
- Documentation
- Information Provided to the HCP
- Identification and Testing of Source Patient's Blood
- Collection and Testing of Employee's Blood
- Counseling
- Post-Exposure Prophylaxis
- Evaluation of Reported Illnesses
- HCP's Written Opinion
- Medical Recordkeeping
Reporting Incident — Employees should immediately report exposure incidents to the employer to permit timely medical follow-up. According to the U.S. Public Health Service, if HIV postexposure prophylaxis is medically indicated it should be initiated promptly, preferably within 1-2 hours after the exposure incident. Immediate reporting also enables the dental employer to evaluate the circumstances surrounding the exposure incident to try to find ways to prevent such a situation from occurring again.
Referral to a Health Care Professional (HCP) — Following a report of an exposure incident, the dental employer shall make immediately available to the exposed employee a confidential medical evaluation and follow-up at no cost to the employee. The dental employer is responsible for providing follow-up, but is not required to perform the follow-up. The employer must refer the exposed employee to a licensed health care professional who will perform all medical evaluations and procedures in accordance with the most current recommendations of the U.S. Public Health Service.
Note: The bloodborne pathogens standard is a performance oriented standard. As such, it requires that medical evaluation and follow-up be provided in accordance with the U.S. Public Health Service recommendations, but does not cite specific recommendations. OSHA intentionally drafted the standard in this fashion to ensure that the most current recommendations would be followed.
Documentation— The dental employer must prepare a report of the exposure incident, including the route(s) of exposure, the circumstances under which the exposure incident occurred, and the identity of the source patient — if known, and if permitted by law (see Identification and Testing of Source Patient's Blood). This report must be placed in the employee's confidential medical record. A copy also must be provided to the evaluating health care professional.
Note: In the past, larger dental practices (those with 11 or more employees) have been required by a separate OSHA record keeping rule (29 CFR 1904) to record occupational illnesses or injuries and prepare an annual log of injuries and illnesses.
Now, all dental practices—regardless of size—are exempt from the record keeping requirements of 29 CFR 1904. The new exemption applies in federal OSHA states to dental offices or clinics, medical offices or clinics and dental and medical laboratories, as well as other workplaces the agency has determined to be low hazard.*
There is one, rare exception to this exemption. OSHA or the Bureau of Labor Statistics may require individual offices to maintain injury and illness records and logs for a year as part of their efforts to gather national injury and illness data. These offices would also have to report their data to the requesting agency. (OSHA Form 300 can be downloaded at http://www.osha.gov/recordkeeping/RKforms.html.)
*Some states operate their own OSHA programs under the authority of a State Plan approved by OSHA. States operating under OSHA-approved plans must have record keeping rules that are substantially identical to the federal requirements. However, they may adopt more stringent requirements. This might include eliminating the exemption for dental offices and other low risk workplaces. Dentists who practice in State Plan states should contact their constituent societies or their state OSHAs for more information about the record keeping requirements in their states.
Information Provided to the HCP — The dental employer must provide the licensed health care professional with a copy of the bloodborne pathogens standard; a description of the employee's job duties as they relate to the incident; a report of the specific exposure incident, including routes of exposure and the circumstances under which exposure occurred; the results of the source patient's blood testing, if available; and relevant employee medical records, including vaccination status, which are the employer's responsibility to maintain. Multiple copies of the standard need not be given to the same health care professional (e.g., if a copy was provided to the health care professional in connection with an earlier exposure incident).
Identification — The employer must identify and document in writing the source patient in an exposure incident, unless this is not feasible or is prohibited by state or local law. The dental employer must contact the source patient, if known, and ask his or her consent to be tested for HBV and HIV infectivity and to disclose the test results to the exposed employee. If consent is not obtained, and is required by local law, the dental employer must document that fact in writing as part of the report of the exposure incident. If consent is obtained, or if it is not legally required and the source patient's blood is available, the source patient's blood must be tested as soon as feasible. The results of the testing must be made available to the exposed employee and he or she must be informed of applicable laws and regulations concerning further disclosure of the identity and infectious status of the source patient.
Note: For those jurisdictions that do not require consent of the patient, the source patient's blood, if available, must be tested. The term "if available" applies to blood samples that have already been drawn from the source patient. OSHA does not require redrawing of blood for HBV and HIV testing without consent of the source patient.
Collection and Testing of Employee's Blood — This section and the following three sections on Counseling, Post-Exposure Prophylaxis, and Evaluation of Reported Illnesses deal with the medical services that must be provided free of charge to an employee who has an exposure incident. The dental employer is required to arrange with a licensed health care professional to provide these services. If the employee consents, the health care professional will, as soon as feasible, collect the exposed employee's blood and conduct baseline testing to establish the employee's HBV and HIV serological status. Baseline testing allows the health care professional to determine whether any subsequently diagnosed disease was acquired as a result of the exposure incident. The employee has the right to decline testing or to delay testing of the collected blood for up to 90 days. If the employee consents to baseline blood collection, but does not give consent for HIV testing at that time, the sample must be preserved for at least 90 days. If, within 90 days of the exposure incident, the employee elects to have the baseline sample tested, such testing shall be done by the health care professional as soon as feasible. The health care professional will notify the employee of all test results. All laboratory tests must be performed by an accredited laboratory at no cost to the employee.
Counseling — Counseling is a vital component of the required post-exposure follow-up procedures. The health care professional will counsel the employee concerning his or her infectious status, including results of and interpretation of all tests, will discuss with the employee the potential risk of infection, and the need for postexposure prophylaxis and the protection of personal contacts.
Post-Exposure Prophylaxis — The licensed health care professional shall prescribe appropriate prophylactic measures, when medically indicated, as recommended by the U.S. Public Health Service. Note: Since post-exposure testing and prophylaxis is a rapidly changing and developing field, it must be provided according to the recommendations of the U.S. Public Health Service current at the time post-exposure testing and prophylaxis take place. The follow-up process may involve multiple visits to the HCP for serial blood tests, monitoring of medications (if prescribed) etc. For example, for employees who have not received the HBV vaccine series, the HBV vaccine (and in some circumstances hepatitis B immune globulin) is to be offered as soon as possible after the exposure incident, but no more than seven days after the incident.
In addition, for HIV, the 1996 CDC guidelines state that "chemoprophylaxis should be recommended to exposed workers after occupational exposures associated with the highest risk of HIV transmission. For exposures with a lower, but non-negligible risk, postexposure prophylaxis should be offered, balancing the lower risk against the use of drugs having uncertain efficacy and toxicity. For exposures with negligible risk, postexposure prophylaxis is not justified."
Evaluation of Reported Illnesses — The health care professional shall also evaluate any reported illnesses of the exposed employee to determine if the symptoms may be related to HBV or HIV infection. This provision ensures that exposed employees will have the benefit of early medical evaluation and recommended treatment and prophylaxis in a timely manner.
Note: This requirement should not be construed to mean that the dental employer is responsible for the cost of treatment of disease, which is beyond the scope of the standard's follow-up requirements.
HCP's Written Opinion — After the health care professional completes the evaluation, he or she is required to send the dental employer a written opinion. The standard requires that the health care professional's written opinion contain only: documentation that the exposed employee was informed of the test results of the evaluation; and the need for further follow-up. If HBV vaccination is provided as part of the post-exposure prophylaxis, the opinion should also state whether HBV vaccine was indicated for the employee and if the employee was vaccinated. All other findings or diagnoses must remain confidential and shall not be included in the written report.
The dental employer must provide a copy of the evaluating health care professional's written opinion to the exposed employee within 15 days of the completion of the evaluation. The original document should be placed in the employee's confidential medical record.
Medical Recordkeeping — The dental employer must establish and maintain medical records in a confidential manner. The standard does not require the employer to maintain possession of the records. If the medical records are left in the possession of the HCP who provides the follow-up protocol, it is the employer's responsibility to arrange with the HCP to maintain and keep the records confidential in accordance with the standard.
Records must be maintained for the duration of employment plus 30 years in accordance with OSHA's standard on Access to Employee Exposure and Medical Records, 29 CFR 1910.20.
Under the standard, dental employers may have to rely on the health care professional to carry out certain OSHA obligations, such as maintaining employee medical records in a confidential manner, retaining the records for the duration of employment plus 30 years and providing appropriate post-exposure evaluation and follow-up services. The dental employer has an obligation to ensure compliance with the standard. However, he or she will not generally be held liable for violations resulting from the health care professional's actions if the dental employer has acted in good faith to contract with a responsible entity and has no reason to foresee that the contractor will not fulfill its obligations.
Prepared by the American Dental Association in cooperation with the Occupational Safety and Health Administration (December 1997). This document is not considered a substitute for any provisions of the Occupational Safety and Health Act of 1970 or for any standards issued by OSHA.
Post-exposure evaluation and follow-up
Questions and Answers for Dental Employers
- Selection of Health Care Professional
- Employer Obligation Related to CDC Recommendations
- Changes to CDC Recommendations
- Confidentiality
- Source Patient Consents
- Medical Records
- Employer Obligation to Former Workers
- Temporary Workers Provided by an Employment Agency
- Potential Patient Anxiety
- Employer Obligation for Medical Treatment
- Responsibility for Obtaining Written Opinion
May the dental employer select the health care professional?
Yes, it is the dental employer, rather than the employee, who is entitled to select a health care professional to provide the hepatitis B vaccination and post-exposure evaluation and follow-up services required under the standard. Dental employers would be wise to select a health care professional who is familiar with the standard and the recommended post-exposure evaluation and follow-up protocol. The U.S. Public Health Service recommends that when possible, the medical evaluation and follow-up should be implemented in consultation with persons having expertise in antiretroviral therapy and HIV transmission. On this basis, the dental employer should identify, and have on record, a health care professional with appropriate expertise, or a healthcare professional who consults with a person having such expertise.
Employer Obligation Related to CDC Recommendations
Since the standard incorporates by reference the CDC recommendations for post-exposure prophylaxis, what is the dental employer's obligations when the CDC guidelines are not clear or when the health care professional recommends treatment beyond what is contained in the CDC guidelines?
Under the standard, it is the dental employer's responsibility, following an exposure incident, to make immediately available to the exposed employee post-exposure prophylaxis, when medically indicated. The standard requires that post-exposure prophylaxis be provided in accordance with the recommendations of the U.S. Public Health Service, but it does not cite specific recommendations.
OSHA intentionally drafted the standard in this fashion to ensure that the most current recommendations would be followed. Because post-exposure testing and prophylaxis are rapidly changing and developing fields, it must be provided according to recommendations of the U.S. Public Health Service current at the time post-exposure testing and prophylaxis take place.
Currently, for employees who have not received the HBV vaccine series, HBV vaccine (and in some circumstances hepatitis B immune globulin) is to be offered as soon as possible after the exposure incident, but no more than seven days after the incident.
With regard to HIV disease, CDC guidelines for post-exposure antiretroviral drug therapy are constantly evolving. The HCP providing post-exposure evaluation and follow-up must ensure that current CDC guidelines are followed. In order to assist the evaluating HCP in following CDC guidelines, the dental employer must ensure that the exposed employee receives immediate post-exposure evaluation (according to the CDC, preferably within 1-2 hours, but no longer than 24 hours) after the exposure incident.
Note: The recommendations of the U.S. Public Health Service provides guidelines for post-exposure chemoprophylaxis. However, the use of post-exposure chemoprophylaxis is a clinical decision which should be individualized for each employee incident.
Changes to CDC Recommendations
How will dentists know of changes in the CDC guidelines that affect their OSHA obligations?
CDC guidelines and recommendations are widely distributed and readily available to health care professionals either directly from the CDC or through professional associations. Direct subscriptions to the Morbidity and Mortality Weekly Report (MMWR) are available. Due to the ever-changing nature of the health care industry, professionals routinely seek to keep themselves abreast of new developments. Therefore, OSHA does not anticipate that either dental employers or evaluating health care professionals will have any difficulty in obtaining any future CDC guidelines or recommendations. (See References.)
Confidentiality
Why is the dental employer denied access to the HBV or HIV test result of the employee and the source patient? How can the dental employer obey state laws implementing CDC guidelines on the practice of infected health care workers if the dentist is not entitled to know the employee's test results following an exposure incident?
It is very important to maintain confidential medical records to ensure that employees report exposure incidents and participate in post-exposure evaluation and follow-up. The standard requires that medical records be kept confidential and not disclosed without the employee's consent, except as required by the standard or as may be required by law. For example, if a law requires the information to be released to a county or state health department, the standard does not prohibit its release.
In addition, the standard does not prohibit the dental employer from providing routine testing of all of his or her employees to determine HBV and HIV status. Such routine testing would enable dental employers to learn the HBV and HIV status of all their employees, not just those few who suffer an exposure incident. Dental employers should be aware, however, that Federal, state or local laws that prohibit discrimination against the disabled may make it illegal to conduct routine employee testing. No dental employer should implement such a program without first obtaining the advice of his or her own personal attorney.
Source Patient Consent
Could the dental employer's obligation to document the identity of the source patient and to provide the source patient's test results to the exposed employee conflict with state confidentiality laws?
The standard requires testing of the source patient's blood for HIV and HBV, and disclosure of the results to the exposed employee, only where it is permitted and not in conflict with applicable laws or regulations. The standard further requires that the exposed employee be informed of any laws or regulations concerning disclosure of the identity and infection status of the source patient. The standard does not, therefore, require dental employers to violate any applicable privacy laws.
Medical Records
May the dental employer make arrangements for the evaluating health care professional to maintain the required confidential employee medical records?
Yes. The bloodborne pathogens standard allows for such arrangements. The dental employer may simply contract with the health care professional who performs the HBV vaccination or post-exposure evaluation and follow-up to maintain the records as part of the service he or she is providing, much like the records that dentists maintain for their own patients. While the standard requires that employers establish and maintain for each employee confidential medical records that include the HBV vaccination status and evaluation and follow-up of exposure incidents, the records need not be kept at the place of employment. The records must, however, be maintained in a manner that makes them accessible to OSHA.
Note: In accordance with OSHA's Standard for Access to Employee Exposure and Medical Records, 29 CFR 1910.1020, employee medical records must be accessible to both the employee (or the employee's representative) and OSHA representatives. To fulfill this obligation, the dental employer must assure that the requestor has the opportunity to examine the relevant employee medical records within a reasonable time (i.e., within 15 working days).
Employer Obligation to Former Workers
What obligation does the dental employer have to pay for post-exposure evaluation and follow-up services after the exposed employee leaves the dentist's employment?
The standard requires the dental employer to make immediately available a confidential medical evaluation and follow-up to an employee reporting an exposure incident. Due to the immediate nature of this requirement, it is not likely that the worker will end his or her employment prior to initiation of the post-exposure evaluation and follow-up. Once an employee ends his or her term of employment, however, the dental employer would no longer be obligated to meet the requirements of the standard since the employer-employee relationship no longer exists. However, employers should be aware that state workers' compensation laws may apply even after the employer-employee relationship ceases.
Temporary Workers Provided by an Employment Agency
When temporary workers are provided through an employment agency, what obligation does the dental employer have to provide post-exposure evaluation and follow-up services?
With regard to temporary workers, all requirements of the standard are applicable. In the case of temporary workers provided through a personnel service, the employer who supplies the workers ("supplying employer") and the client facility to which they supply workers ("using employer") have a shared responsibility to ensure that workers are protected from workplace hazards. The supplying employer, who maintains the continuing relationship with the workers, is required to ensure that all workers are provided with the required vaccinations and follow-up evaluations. The using employer will not be held responsible for providing the required vaccinations and follow-up evaluations unless the contract specifies that the using employer will do so.
Potential Patient Anxiety
The standard requires source patient testing, if feasible, following an exposure incident. Couldn't this requirement interfere with the doctor-patient relationship and cause patient anxiety due to possible misinterpretation of the request (i.e., that the patient rather than the employee has been potentially exposed)?
Testing of the source patient whenever possible is very important to minimize the anxiety employees experience after exposure incidents. Testing for a source patient's infectious status provides exposed employees with information that will assist them in decisions regarding testing of their own blood, complying with other elements of post-exposure management, and using precautions to prevent transmission to personal contacts. In addition, such testing assists the health care professional in deciding on appropriate follow-up.
We recognize that some dentists may have concerns about potential patient fears; however, we note that the standard is designed to prevent occupational exposure to blood or OPIM and, if properly implemented, exposure incidents will be uncommon events. If an exposure incident does occur, much can be done to eliminate or reduce patient anxiety. Medical professionals must often convey sensitive or unpleasant information to patients and have learned to do so without unduly alarming patients.
For example, when a health care professional treats a patient in a dental office or in any other medical setting, he or she typically explains office procedures and policies to the patient prior to providing services. OSHA suggests that as a part of this discussion, it would be appropriate for the dental employer to explain the standard's requirements for source patient testing to determine if the employee has been exposed. Thoroughly discussing this issue prior to, or at the time of, an exposure incident will likely reduce patient anxiety and possible misunderstandings.
Employer Obligation for Medical Treatment
What obligation does the dental employer have to pay for medical treatment of a disease acquired as a result of an exposure incident?
The standard requires the employer to make available testing, post-exposure prophylaxis (when medically indicated), counseling and evaluation of reported illnesses. Treatment of disease is beyond the scope of the standard's follow-up requirements. (Treatment of disease is generally handled under workers' compensation or other disability insurance.)
Responsibility for Obtaining Written Opinion
What happens if the health care professional fails to provide a written opinion as required by the standard? Might the dental employer be held responsible?
As noted previously, the dental employer may have to rely on the health care professional to carry out certain OSHA obligations, such as providing appropriate post-exposure evaluation and follow-up services, including providing a written opinion to the dental employer. The dental employer is responsible for providing the health care professional with pertinent information (see Information Provided to the HCP and Flow Chart). In particular, the dental employer must ensure that the health care professional understands the requirements of the standard and agrees to comply.
It remains, however, the dental employer's obligation to ensure that he or she obtains and provides the exposed employee with a copy of the health care professional's written opinion. Failure of the dental employer to obtain the written opinion generally constitutes a violation of the standard. However, the dental employer will not generally be held liable for such violations if the dental employer can demonstrate good faith efforts to obtain the written opinion (i.e., by documented phone calls or written communication to the health care professional). In this way, the dental employer shows that he or she clearly tried to comply with the intent of the standard, and a violation may not exist.
Reference
OSHA
- Occupational Exposure to Bloodborne Pathogens 29 CFR 1910.1030
- All About OSHA (2006)
- Access to Medical and Exposure Records (2002)
Centers for Disease Control and Prevention (CDC)
- Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings MMWR September 22, 2006; Vol 55, No RR14
- Updated US Public Health Service Guidelines for the Management of Occupational Exposures to HIV and Recommendations for Post-exposure Prophylaxis MMWR September 30, 2005; Vol. 54, No RR9;1
- Immunization of Health-Care Workers MMWR December 26, 1997; Vol 46, No RR18
- Influenza Vaccination of Health-Care Personnel MMWR February 24, 2006; Vol 55, No RR2;1
Additional Links
By linking to other Websites, the ADA does not endorse the policies or practices of, or opinions expressed on, those sites; nor does the ADA make any representations or warranties with respect to the accuracy of any items or claims contained therein.
- American Medical Association
- Centers for Disease Control and Prevention
- HIVdent
- Morbidity and Mortality Weekly Report
- National Institute of Dental and Craniofacial Research (NIDCR)
- National Institutes of Health (NIH)
- National Library of Medicine (NLM)
- Occupational Safety and Health Administration (OSHA)